Shenyang (China), Jul 13: China's Nobel laureate Liu Xiaobo died today while still in custody following a battle with cancer, authorities said, after officials ignored international pleas to let him spend his final days free and abroad.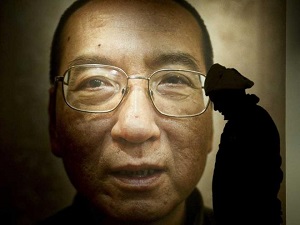
The prominent democracy advocate died aged 61, more than a month after he was transferred from prison to a heavily- guarded hospital to be treated for late-stage liver cancer.
The legal bureau in the northeastern city of Shenyang said on its website that Liu died three days after going into intensive care at the First Hospital of China Medical University.
The writer's death silences a government critic who had been a thorn in the side of the authorities for decades and became a symbol of Beijing's growing crackdown on dissenting voices.
Liu's death puts China in dubious company as he became the first Nobel Peace Prize laureate to die in custody since German pacifist Carl von Ossietzky, who passed away in a hospital while held by the Nazis in 1938.
International human rights groups, Western governments and local activists had urged authorities to free Liu and grant his final wish to be treated abroad.
Germany had offered to treat Liu, calling for a "signal of humanity" from China. The United States also said it was willing to take him in.
But officials insisted that Liu was receiving treatment from top Chinese doctors since being granted medical parole following his diagnosis in late May.
In response to calls to allow Liu to leave China, the foreign ministry repeatedly said other countries should not interfere in China's internal affairs.
In early July, Liu's Chinese doctors said he was not healthy enough to be sent abroad for treatment, a position that was contradicted by US and German medical experts invited by the hospital to examine Liu's condition. The physicians offered to treat the laureate at hospitals in their home countries.
Human rights groups decried the way the government treated Liu, accusing authorities of manipulating information about his health and refusing to let him leave because they were afraid he would use the freedom to denounce China's one- party Communist regime.
As a gaunt Liu lay in his sickbed, a video was leaked showing the Western doctors praising their Chinese counterparts -- a scene that was denounced as "grotesque propaganda" by Human Rights Watch.
The German embassy said the video seemed to show that security organs were "steering the process, not medical experts".
Liu was arrested in 2008 after co-writing Charter 08, a bold petition that called for the protection of basic human rights and reform of China's political system.
He was sentenced to 11 years in prison in December 2009 for "subversion". At the Nobel Peace Prize ceremony in Oslo in 2010 he was represented by an empty chair.
Liu is also known for his role in the 1989 Tiananmen Square protests in Beijing.
His wife, Liu Xia, was placed under house arrest in 2010, but she was allowed to see him at the hospital. Her fate will now worry human rights groups, which had urged the government to free her alongside Liu Xiaobo.





Comments
Add new comment